Telehealth Coding & Billing Guide
WHAT IS TELEMEDICINE?
The WHO defines telemedicine as:
“The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities”
While telemedicine refers specifically to remote clinical services, telehealth can refer to remote non-clinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
HOW DOES REIMBURSEMENT WORK FOR TELEHEALTH SERVICES ?
Reimbursement is dependent on your State, payer coverage, and patients’ coverage with their insurance providers. This document is intended to provide a broad-strokes guide to telehealth reimbursement across all 50-states, with regard to Medicare reimbursement, and with some regard to new updates after the COVID-19 outbreak.
We encourage all practices to verify with their state and individual payers to get more specific information about how payers will individually reimburse for telehealth services.
GENERAL CONSIDERATIONS
- Understand the coverage and reimbursement rules from your patients insurance, including Medicare beneficiaries
- Insurance policies may have certain limitations on coverage around telemedicine
- Eligible providers may be also limited
- Location of the patient may also be a limiting factor on coverage and reimbursement
- CareCloud’s eligibility tool, payer portals, and telephone coverage/reimbursement eligibility tools can help in understanding your patients coverage/reimbursement for telemedicine
- Providers should contact their provider representative as this service might need to be added to their existing contracts. Please note, coverage and reimbursement varies from plan to plan, even within the same insurance company.
HANDLING TELEHEALTH WITH IN-NETWORK PAYERS
There are a number of scenarios that could exist with payers you are contracted with:
- The patient carries a health plan with a payer that covers telemedicine:
- We suggest you call the payer to assess the extent of coverage for telehealth services for this plan. Always remember to document the conversation, ask the representative’s name and ask for a call reference number.
- Some questions we suggest asking in assessing coverage by commercial payers:
- Are the CPT codes covered (be explicit and clear on the CPT codes for the service, i.e. 99441-99443)?
- Would E/M codes be covered with GT, GO, 95 modifiers?
- Would it be preferred to identified telehealth services by using the appropriate modifier or will the POS 02 be sufficient (validate this information with the providers medicare jurisdiction )
- If the answer is yes on above, ask if authorization is required for the services.
- Are there any caps on telemedicine services for the patient’s benefit plan?
- Does the reimbursement rate for the services differ or equal from an in-person visit?
- Are there any specific documentations and/or notes that must be included on the when documenting the telemedicine visit?
- Does the patient have any out of pocket expenses? (please review link on HHS/OIG Policy about the Stark Law requirements)
- Finally, skip to the How To Bill Telehealth Services section below.
- The patient’s health plan or the payer does not support or cover telemedicine. You have a few options:
- Treat the patient as uncovered or self-pay. see Out-of-Network Payers, Non-Covered Service or Self Pay patients section below.
- We suggest you nonetheless call the payer, and ask for an exception in light of the COVID-19 outbreak. In this case, follow the steps above to document the conversation.
- When calling the payer:
- Document the conversation
- Ask for the representative’s name
- Request a call reference number. This may help in disputing any denials for coverage.
- If the payer agrees to provide coverage:
- Some payers may ask you to fill out and sign an approval form.
- Follow any other instructions the payer provides and document them.
- When calling the payer:
HANDLING TELEHEALTH FOR OUT-OF-NETWORK PAYERS, NON-COVERED SERVICES, OR SELF-PAY PATIENTS
In the case that you are providing services to non-covered plans, and the patients insurer has refused to cover telehealth, you should treat patients as self-pay:
- Have the patient sign a consent of financial responsibility (i.e. ABN)
- Breeze users: Create Financial Responsibility form in Breeze to send out to your patients via Breeze
- Collect fees up front based on your fee schedule
- Use your merchant account of choice to store and collect fees
- CareCloud Breeze users can use the card on file feature, execute payment plans, or charge up front for the services
- Use your merchant account of preference to collect and track your payments
- Once you have assessed all of the above, then move to How to bill for Telehelath.
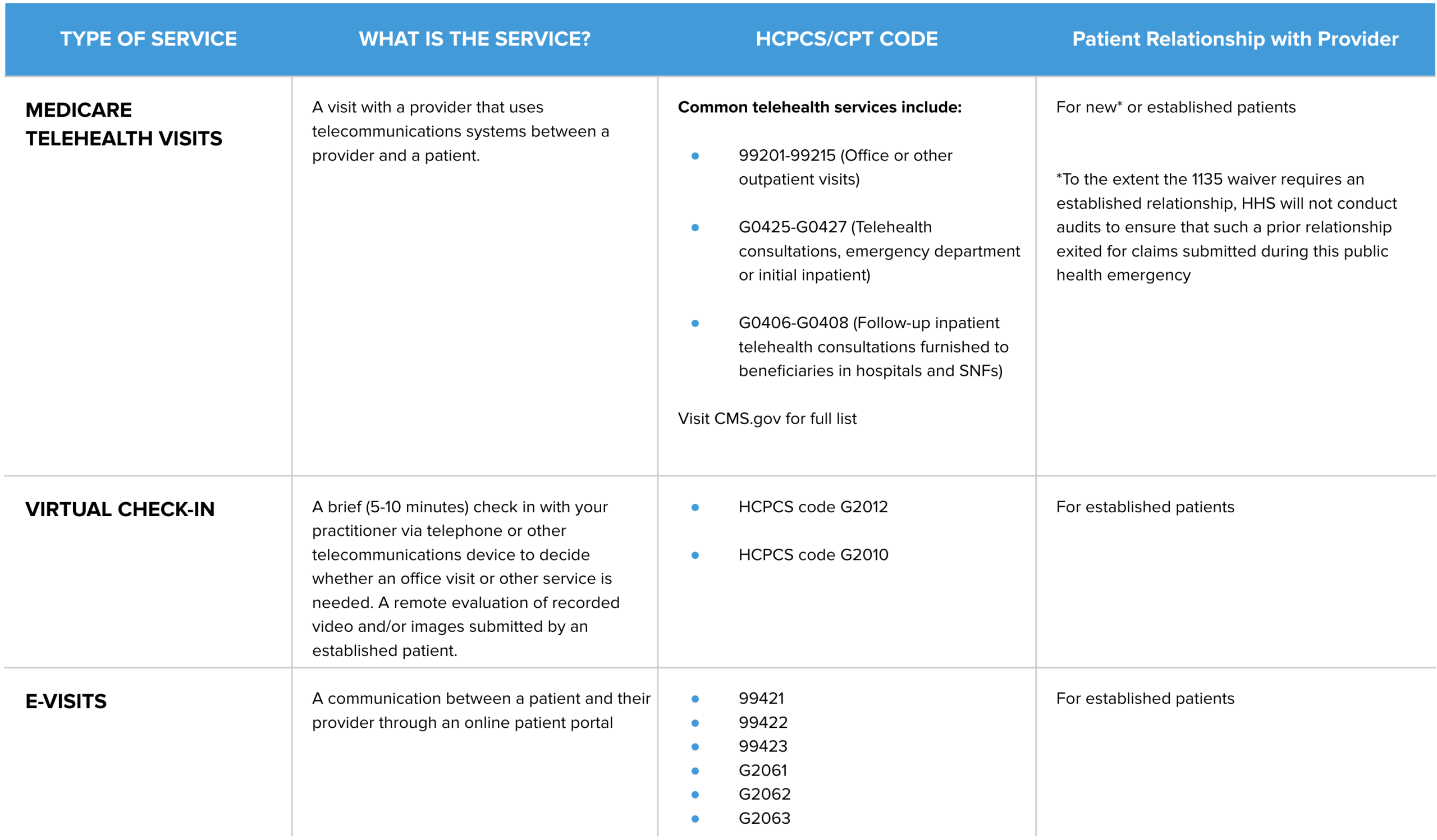
HOW TO BILL FOR TELEHEALTH SERVICES
Place of service (POS):
- 02 Telehealth: The location where health services and health related services are provided or received, through a telecommunication system.
In regular circumstances Medicare, Medicaid or Children’s Health Insurance Program (CHIP) would require providers to meet specific criterias in order to be reimbursed for any telehealth/telemedicine services. However, most of these requirements have been waived due to the declaration of public health emergency and since then established 1135 waivers. Examples of these 1135 waivers or modifications include allowing providers to bill and get reimbursed for regular Evaluation and Management (E/M) codes ( see below ) with a POS 02 in place of the regular telehealth codes. Therefore, E/M codes and Telehealth codes are both accepted forms of reporting Telehealth services.
CPT codes:
- Appropriate Evaluation and Management CPT codes
-
- New Patients: 99201- 99205
- Established Patients: 99211- 99215
- Telephone Evaluation and Management CPT codes
-
- 99441-99443: Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment
- Virtual Check- in code range G2010-G2012
-
- G2010 : Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment
- G2012 : Brief communication technology-based service, e.g., virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion
Modifiers:
- GT : Via interactive audio and video telecommunication systems
- GO : Telehealth services for diagnosis, evaluation, or treatment, of symptoms of an acute stroke.
- 95 : Synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. Append this modifier to an appropriate CPT code (listed in Appendix P in the CPT manual) for a real time interaction between a physician or other qualified healthcare professional and a patient who is located at a distant site from the reporting provider.
Documentation Integrity
- Total time spent should be documented on Physician’s note.
- In the virtual environment, Level 3 and 4 reimbursements must be based on time rather than physical examinations a. Providers should document the length of time of the consultation visit and should note that more than 50 percent of the encounter was spent counseling/coordinating care.
- Documentation should include: differential diagnosis, active diagnosis, prognosis, risks, benefits of treatment, instruction, compliance, risk reduction, and coordination of care with other providers.
- Documentation under HPI must provide information on who initiated the services example: “ Telephone services initiated by patients for today’s date of service”. This information should be documented under the HPI portion of the note.
- Lastly, Telemedicine consultation documentation must meet the same standards as a face-to-face encounter.
WEBSITES AND RESOURCES
Please note that as further updates develop, some of the information within this document may change. States and Payers may make changes/updates as necessary.